Published By BHF | November 18, 2022

Starting August 2022, Busoga Health Forum played a co-host of three resident pediatricians from Astrid Lindgren Children’s Hospital at Karolinska University Hospital in Stockholm, Sweden. They were received and ushered into Jinja Regional Referral Hospital.
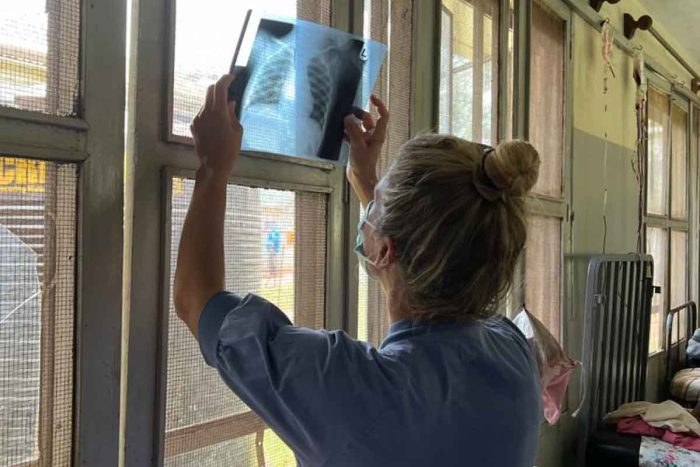
In this exchange program of Jinja Regional Referral Hospital with Astrid Lindgren Children’s Hospital, Dr Fredrik Fahnehjelm, Dr Cecilia Fahnehjelm and Dr Emma Hernstrōm explored ways to improve quality of care in areas affecting child health with specific focus on neonates, children with developmental delays/impairment and children in need of emergency/critical care.
It’s been about six weeks at the hospital, and Claire Zerida Balungi caught up with them in a chat.
Claire:
What’s it been like so far?
Cecilia:
We’ve had a real time here. We feel we are learning a lot every day even though it is also hard most days since everything is still new but we have been talking amongst ourselves and we all agree that the people here have been so warm and helpful which has made us feel welcome and helped us contribute.
Fredrik:
We had a bit of a threshold to begin with because of the language problem and the new diseases we don’t know anything about like Malaria, Sickle Cell disease amongst other things, that I feel when we managed to get abreast with those diseases, we are now contributing especially since the new interns from Ugandan universities came. Usually the hospital hosts interns for six months. At the beginning of our rotation the old interns had been here for about five months so they were really skilled and knew pretty much. We have received new ones and they are quite fresh. We are learning as we help them acclimatize to the pediatric ward and the Special Care Unit (SCU) and we’re working as a team so am thinking it’s been good that we have been there for them. Sometimes the introduction for the new interns is scarce.

Emma;
We read a lot about the new diseases and I’m now able to contribute at the Malnutrition Ward. The interns are helping us a lot with things that are different from the Swedish context. You learn to adapt and be a little bit more creative than we are used to in Sweden.
Cecilia;
If there’s anything to learn in Uganda, it’s to be creative. When there is need to give medicine that is either too expensive or not in the hospital pharmacy, we have then to look for another option that has to work. We then talk to many people like other doctors to just get it right.
Fredrik;
One thing I did today was; we had a preterm (baby born premature) who was way too cold and one way to heat them up is to put them in a plastic bag. The only thing I could find was the little plastic bag that had face masks, so I took the face masks out and used that piece of plastic to cover the child. We managed to get the temperature a bit at least. That’s something I learnt from Sister Maburuka Anguparu, a Senior Nursing Officer, two weeks ago.

Claire;
I suppose it would be easy for you to work in a slightly similar setting to Uganda’s, seeing as you’ve gathered some special experience.
Cecilia;
It would be easy for us to work in a slightly different setting in Africa similar to Uganda’s. For one, we’ve learned about Malaria and other tropical diseases. We have learnt not to be limited by boundaries like scarcity of logistics. Perhaps back home we have more rules and boundaries, but here and in other settings all over Africa, we’d manage.
Claire;
Have you had to consider taking any shortcuts due to scarcity of resources?
Emma;
Regarding the use of phototherapy in the SCU (Special Care Unit)back home, we would only use one phototherapy machine for one child and that’s also for hygienic reasons, we don’t want any bacteria to spread, but here we need to take a shortcut, skip the hygiene part and put two or three babies in the same machine since they are scarce. That’s riskier. That would be an example of a shortcut.
Fredrik;
Sometimes you have to limit your time and instead of taking a blood sample and do a perfect clinical assessment for only three kids out of ten, leaving seven unattended by the doctor, you could do everything not 100%. Instead of giving three kids 100% and seven kids 0%, you give all the ten kids 80%. We’ve learned to give good enough instead of best all the time because in that way you can help a lot more kids.
Emma;
I agree with Fredrik. Doing everything 100% isn’t always the best fit. Sometimes we go into details in a way that isn’t the best for the kids and doing a lot of extra analysis or over diagnostic isn’t best.
Cecilia;
We are practicing on just doing the right amount of examination. Back home, it’s always easy to send the request to assess a blood sample even though you don’t need it, unlike here where the sample could take a lot of time in the lab.
Fredrik;
And also, we have to trust our clinical assessment more. Back home, we do a clinical assessment and then we also do the tests but here we don’t have that opportunity so we have to be better at our clinical assessment and trust it. And trusting our assessment is something that involves us, being doctors.
Emma;
In Sweden, it’s important to think about the cost even though one does not pay for the blood samples and investigations. It takes more knowledge to start thinking about what you are actually subjecting a patient to, as a doctor, and what the costs are.
Cecilia;
It’s about being considerate. Even though the children in Sweden don’t pay for the lab results, they pay with pain and with radiation, so we should restrict.
Claire;
Creativity, have you applied that sense of creativity to other parts of your life?
Fredrik;
I made my own coffee maker out of a plastic bottle.
Claire;
How have you engaged with the hospital community and its close beyond?
Fredrik;
Like Cecilia said, we’re really liking the people and one thing for us staying here for six weeks is that we have gotten to know the old interns so we need them at the OBS GYN ward and at the surgical ward. On the streets, the kids at the restaurant know us and one of them fell in love with Emma. She chases her all the time.
One thing I thought was really funny was the guy who has a restaurant just outside the hospital. Usually back home we eat at 12 O’clock. The first two weeks I came to him at 12 O’clock asking for lunch, he said, “You have to wait two more hours. We have lunch at 2pm. But tomorrow I will fix something for you at 12 O’clock. For a couple of days, he actually had lunch for me at 12 O’clock but then one day we worked late so I came at 4pm and they at the restaurant wondered where I had been. I said sorry and told them I’d been working late at the hospital. The gentleman looked at me and said, “Okay, now you’re an African” because I was late. (giggles)
Cecilia;
At the hospital, I would say, we are spending a lot of time with the nursing students. They are the ones translating for us. It’s very important for us to have a good relationship with them. I think we have some great knowledge-sharing moments during those rounds. As they translate, I think they learn a lot in the process.
Emma;
We spend almost all our time at the hospital so after being at the hospital, we go home to study.
(interrupts Fredrick)
Or go for a run. Cecilia brought some ingredients for Swedish pastry so we’ve been watering our mouths.

Claire;
What are you most proud of in this journey?
Fredrik;
Something that I felt really proud of was when one of the medical students told William, who is in charge of the students’ Medical Program, that the medical students said that they felt very at ease when they were with us. They can ask questions so if there is something that they don’t know they just hope that their senior/ the Doctor isn’t going to ask them about it as they may not have the knowledge, but with us, it is the opposite, they feel encouraged to ask questions while we teach them. That it is a good thing as they get to learn a lot more and look up to us, feel free to ask instead of being fearful of their superiors. That way of working is something that, I’m sure, reflects on them and when they are doctors they are going to be great instructors to their medical students and encourage them to ask questions and learn more.
Emma;
Fredrik also had a lecture about Communication especially in key emergency situations. I think that’s something to implement in this kind of setting. It’s important to have good and safe communication; Safe communication is a concept from the Civil Aviation industry which recognizes that the industry has a lot of accidents and it’s barely due to lack of knowledge but because of poor communication. For example in the theatre, if a doctor wants something to be done, the other person should confirm that they are going do it and then when they acknowledge, they should let the doctor know so that the doctor is sure that the ones they are talking to know that they are being talked to. Safe communication takes the form of naming, gestures and more. It is a part of the things one can do to make it safer in the hospital setting. Not being afraid of asking is also part of it. You feel safe in the environment you are in and if you see something, don’t feel afraid to tell a superior what’s happening.
Cecilia;
Yesterday I had a tough situation with a patient. It was very hard to communicate with the parents of the patient. It took so long just to understand why the child was there. A nurse who spoke Lusoga had to intervene. I’m proud that I was patient about the situation.
Emma;
We are able to teach and both learn about the very many things we don’t know especially concerning new diseases. It’s the small things you are proud of, it’s a developmental curve and we’re grateful that our colleagues always figure out a way to make it better for us.
Fredrik and Emma;
The Jinja-Stockholm project will be on for some years. Since we’re here, we can see the challenges so we can make it easier for our colleagues next time.




